I really did get breast implants for myself. I never changed from my day to day tank tops I've always wore. I never wanted to show them off. I suppose my wedding day when I got remarried was one time I did. I was a 32 D then and I'd never regretted my decision. I was actually really happy to share my confidence with my body with my second husband. But when I became pregnant with my third daughter, I'd realized something was changing. Did you know that breast implants can come with a complication called "capsular contracture" ? |
| This time, I had years of education, years of experience helping nearly 90 women birth by their side. AND I had a husband who loved me tremendously that I trusted more than anyone else. This time, I was hell bent on homebirth. I started to say "hospital birth was no place for a low-risk mom and baby." Which, is still basically true in my mind. But what I didn't realize I meant was "I'm angry at all the coercion and abuse I've witnessed for my doula clients." I also didn't realize I'd developed a complete IDOL in midwives and homebirth. It was difficult for it to be about the baby and me. It was all about that standard of care. And therefore, my third birth became a performance. |

I had no idea I would feel so pressured. Make no mistake, it was of no fault of the midwives. It was completely self-driven. I anticipated feeling performance for my students, but not for my birth team. I knew I had to surrender to what the hundreds of students and doula clients may think of this birth. But I didn't know I was looking at midwives on an even higher pedestal.
My water released at 12:30am on November 3rd. By now, I'd spent years telling women to go back to sleep when this happens and not to get too excited. All that teaching paid off for myself. Ironically, this is exactly how my first birth started only, all the adrenalin in the world rushed in. This time I calmly texted my husband who was at work. And we both tried our best to sleep that night when he got home a little while later. I set up the bed with the "toss away" sheets and got myself more ready for the birth so I could sleep peacefully while I went to the bathroom many times leaking BUCKETS of water. I did have some waves (contractions) but nothing too much. Just enough to make a little sleep difficult, but doable. That next day was calm for the most part.
We walked to the chiropractor (only a mile away) as I'd been dealing with massive rib pain for weeks and I didn't know why. I figured one last adjustment might help the rib pain be more tolerable for the birth. We also walked to the grocery store and bought more pads since I was going through all that I'd bought for the postpartum use! I was leaking SO much. The waves would come and go and got stronger a bit after the walk so my midwife came over.
I don't remember exactly when. I think it was the second time she came over that day. But on her way, I started crying and told Josh I'd rather just birth with no one there. But I knew that kind of birth was WAY off his radar. That wasn't something we'd ever talked about. So I knew that just wasn't going to happen. A dear friend Stephanie came over and hugged me and lent me a breast pump to try and get more waves. I was upset that I had put my midwife out of her regular schedule for a whole day. I felt TONS of completely self-induced pressure to have a baby faster just for the people involved. My videographer was aware my water released and waiting, my friend and doula was aware and waiting. The student midwives were also on call. The more I thought about another person, the more my waves would disappear. And meanwhile, the rib pain grew and grew.
The next night came and I was more relaxed. As I got a bit of broken sleep through more waves, I was more prepared for an inevitable birth that next day. It was just statistically more likely, so I figured I wouldn't be bothering people waiting for active progression for too long. At one point during the night, my waves picked up a LOT. All of the sudden I was shaking and vomiting. But then, all my waves went away! It was the strangest thing. But looking back, I wonder if the rib pain was also a block in progression on top of my own brain being in the way. We found out when Anaiah was born her foot must have been jammed under my ribs in some way, her little ankle was totally contorted from it.
Anyways, the morning came and a different midwife came over. I wasn't upset I didn't have the midwife I planned to be with. I really adore all of them! .But as the day went on, the rib pain grew, and the waves came and went like a roller coaster. I tried castor oil which was a big mistake I think now. I had no idea what I was doing with that! I probably took too much and it probably dehydrated me. I didn't even know much about what to expect with it, I just figured it was best to try everything instead of wishing I did. But what conflicting thoughts I had! On one hand I said "oh it'll happen today," and on the other hand "I better try everything." I know you cannot hold two conflicting thoughts within your mind at the same time. This was a problem. I needed to value myself and my baby and just listen to THAT voice of instincts from THAT place! But it's hard to value yourself when you're idealizing people around you.
I really had ZERO pain with every single wave. All of the physical process of birthing I got to experience at home was absolutely amazing! I LOVED all my surges completely. But I HATED the rib pain. Why couldn't I figure out what was causing it? Why did the massage make it worse? Why was nothing getting rid of it completely. I started to became really mad at it. To the point where I was biter at God. But all of the sudden, I was hit with a big realization. Even if I couldn't figure out why I had this horrible pain, or how to get rid of it completely, Even if it made my birth different than I'd plan. That is SUCH a small thing to surrender. I can do that for my baby! I started crying a lot as I broke through that barrier. It was a great release! By the late afternoon I asked to have my cervix checked. I was 5cm open, 80% thinned, and baby was at a -1 station. None of this was told to me, when I learned it later, I was very surprised. I didn't think I had any real waves to get me to that point!
The time past became a bigger source of anxiety again as the day became evening. And I was really upset that someone had asked the videographer to come because I DID NOT think I was in any kind of labor at all yet. Finally, I asked my husband and when he told me I was 5cm, I was more encouraged to move around as my birth team encouraged me despite how tired I was.
This is when I got to experience at least on little progression I wanted. I got in the birth tub. IT WAS BLISS!!!! Not only was I in love with my waves, but NOW I was rid of the rib pain in the water enough to really move with them too! I LOVED THIS WATER like nothing I could ever describe. It was pure heaven. I began to see myself birthing there and even said to myself, "I'm supposed to birth here."
BUT as my waves grew, my team encouraged me verbally more. And unfortunately, their well intentioned efforts were strangely a source of more pressure. I didn't need anyone to say anything. I was in perfect peace. When I would hear their voices, I was aware of their presence, and that was a problem for my pattern to progress more.
click on this picture below to see my birth video
My water released at 12:30am on November 3rd. By now, I'd spent years telling women to go back to sleep when this happens and not to get too excited. All that teaching paid off for myself. Ironically, this is exactly how my first birth started only, all the adrenalin in the world rushed in. This time I calmly texted my husband who was at work. And we both tried our best to sleep that night when he got home a little while later. I set up the bed with the "toss away" sheets and got myself more ready for the birth so I could sleep peacefully while I went to the bathroom many times leaking BUCKETS of water. I did have some waves (contractions) but nothing too much. Just enough to make a little sleep difficult, but doable. That next day was calm for the most part.
We walked to the chiropractor (only a mile away) as I'd been dealing with massive rib pain for weeks and I didn't know why. I figured one last adjustment might help the rib pain be more tolerable for the birth. We also walked to the grocery store and bought more pads since I was going through all that I'd bought for the postpartum use! I was leaking SO much. The waves would come and go and got stronger a bit after the walk so my midwife came over.
I don't remember exactly when. I think it was the second time she came over that day. But on her way, I started crying and told Josh I'd rather just birth with no one there. But I knew that kind of birth was WAY off his radar. That wasn't something we'd ever talked about. So I knew that just wasn't going to happen. A dear friend Stephanie came over and hugged me and lent me a breast pump to try and get more waves. I was upset that I had put my midwife out of her regular schedule for a whole day. I felt TONS of completely self-induced pressure to have a baby faster just for the people involved. My videographer was aware my water released and waiting, my friend and doula was aware and waiting. The student midwives were also on call. The more I thought about another person, the more my waves would disappear. And meanwhile, the rib pain grew and grew.
The next night came and I was more relaxed. As I got a bit of broken sleep through more waves, I was more prepared for an inevitable birth that next day. It was just statistically more likely, so I figured I wouldn't be bothering people waiting for active progression for too long. At one point during the night, my waves picked up a LOT. All of the sudden I was shaking and vomiting. But then, all my waves went away! It was the strangest thing. But looking back, I wonder if the rib pain was also a block in progression on top of my own brain being in the way. We found out when Anaiah was born her foot must have been jammed under my ribs in some way, her little ankle was totally contorted from it.
Anyways, the morning came and a different midwife came over. I wasn't upset I didn't have the midwife I planned to be with. I really adore all of them! .But as the day went on, the rib pain grew, and the waves came and went like a roller coaster. I tried castor oil which was a big mistake I think now. I had no idea what I was doing with that! I probably took too much and it probably dehydrated me. I didn't even know much about what to expect with it, I just figured it was best to try everything instead of wishing I did. But what conflicting thoughts I had! On one hand I said "oh it'll happen today," and on the other hand "I better try everything." I know you cannot hold two conflicting thoughts within your mind at the same time. This was a problem. I needed to value myself and my baby and just listen to THAT voice of instincts from THAT place! But it's hard to value yourself when you're idealizing people around you.
I really had ZERO pain with every single wave. All of the physical process of birthing I got to experience at home was absolutely amazing! I LOVED all my surges completely. But I HATED the rib pain. Why couldn't I figure out what was causing it? Why did the massage make it worse? Why was nothing getting rid of it completely. I started to became really mad at it. To the point where I was biter at God. But all of the sudden, I was hit with a big realization. Even if I couldn't figure out why I had this horrible pain, or how to get rid of it completely, Even if it made my birth different than I'd plan. That is SUCH a small thing to surrender. I can do that for my baby! I started crying a lot as I broke through that barrier. It was a great release! By the late afternoon I asked to have my cervix checked. I was 5cm open, 80% thinned, and baby was at a -1 station. None of this was told to me, when I learned it later, I was very surprised. I didn't think I had any real waves to get me to that point!
The time past became a bigger source of anxiety again as the day became evening. And I was really upset that someone had asked the videographer to come because I DID NOT think I was in any kind of labor at all yet. Finally, I asked my husband and when he told me I was 5cm, I was more encouraged to move around as my birth team encouraged me despite how tired I was.
This is when I got to experience at least on little progression I wanted. I got in the birth tub. IT WAS BLISS!!!! Not only was I in love with my waves, but NOW I was rid of the rib pain in the water enough to really move with them too! I LOVED THIS WATER like nothing I could ever describe. It was pure heaven. I began to see myself birthing there and even said to myself, "I'm supposed to birth here."
BUT as my waves grew, my team encouraged me verbally more. And unfortunately, their well intentioned efforts were strangely a source of more pressure. I didn't need anyone to say anything. I was in perfect peace. When I would hear their voices, I was aware of their presence, and that was a problem for my pattern to progress more.
click on this picture below to see my birth video
There were more "problems" arising. My baby's heart rate crept up from a normal baseline in the 140s to the 160s and then reaching the 180s with no variables. Also, I began to develop a fever that crept up to 102. I was mildly aware of these things even though no one was telling me. But when we did another long listen to her heart rate, and I heard the numbers called out by the student midwives, I knew exactly what needed to happen.
Even before they were finished, I said to Josh, "we're transferring, this is too many signs of infection." Now nearing 48 hours of my water being released we were on our way to the hospital. Transferring from a homebirth was FAR off my radar. I had no idea this would happen to me. I'd already given birth unmedicated before. I'd already had two vaginal births. The concept of transferring had only crossed my mind as an extreme emergency in the absolute most rare of circumstances.
When I got out of the car and walked through the emergency room doors. I went into a completely different place mentally as well. I was very worried for my baby, but I was also walking into a battleground in warrior mode. My attitude towards the hospital staff compared to the midwives at home was night and day. At home, I was making jokes and wouldn't ask them for things. At the hospital I made no eye contact, completely ignored everyone and focused on what my baby and my body needed ONLY. What anyone else needed was out of my thoughts completely. Now it was ONLY about me and my baby. This is the attitude I needed at home.
My waves got closer and stronger then ever. The castor oil was taking full effect and I had to make many trips to the bathroom with much discomfort from that. The nurse checked me and she said I was 3cm. This was a blow. Before this information, I told myself "it's fine, I'll get antibiotics and a little bit of Pitocin and I'll have my baby in a few hours or less." Not now. Now I was facing the third night of no sleep and the Pitocin was getting turned up more and more and more. I tried to stay positive, but I totally lost my zone. I was not composed anymore. I was facing PANIC mode 100%. I became tense from head to toe. This was the fear tension pain syndrome in full effect.
I'd asked to be checked. It had been a few hours and I was just 4cm now. I was done. All plans were out the window. I was in the WORST pain. I knew this was not going to work like this all night. Even though I was terrified of another injury from it, I asked for an epidural. Knowing now that the baby was fine, her heart rate had totally settled and my temperature was back down. I said I'm either going back home or I'm getting an epidural. Again, I knew no one was going to take me home. But OH how I wish that I could've. It's never fun to have to share a story as a natural childbirth educator that you got an epidural.
The anesthesiologist walked in and I barked orders at him with the 30 seconds to spare between ROARING in waves.
Even before they were finished, I said to Josh, "we're transferring, this is too many signs of infection." Now nearing 48 hours of my water being released we were on our way to the hospital. Transferring from a homebirth was FAR off my radar. I had no idea this would happen to me. I'd already given birth unmedicated before. I'd already had two vaginal births. The concept of transferring had only crossed my mind as an extreme emergency in the absolute most rare of circumstances.
When I got out of the car and walked through the emergency room doors. I went into a completely different place mentally as well. I was very worried for my baby, but I was also walking into a battleground in warrior mode. My attitude towards the hospital staff compared to the midwives at home was night and day. At home, I was making jokes and wouldn't ask them for things. At the hospital I made no eye contact, completely ignored everyone and focused on what my baby and my body needed ONLY. What anyone else needed was out of my thoughts completely. Now it was ONLY about me and my baby. This is the attitude I needed at home.
My waves got closer and stronger then ever. The castor oil was taking full effect and I had to make many trips to the bathroom with much discomfort from that. The nurse checked me and she said I was 3cm. This was a blow. Before this information, I told myself "it's fine, I'll get antibiotics and a little bit of Pitocin and I'll have my baby in a few hours or less." Not now. Now I was facing the third night of no sleep and the Pitocin was getting turned up more and more and more. I tried to stay positive, but I totally lost my zone. I was not composed anymore. I was facing PANIC mode 100%. I became tense from head to toe. This was the fear tension pain syndrome in full effect.
I'd asked to be checked. It had been a few hours and I was just 4cm now. I was done. All plans were out the window. I was in the WORST pain. I knew this was not going to work like this all night. Even though I was terrified of another injury from it, I asked for an epidural. Knowing now that the baby was fine, her heart rate had totally settled and my temperature was back down. I said I'm either going back home or I'm getting an epidural. Again, I knew no one was going to take me home. But OH how I wish that I could've. It's never fun to have to share a story as a natural childbirth educator that you got an epidural.
The anesthesiologist walked in and I barked orders at him with the 30 seconds to spare between ROARING in waves.
| Now EVERYTHING I envisioned for this birth was gone. (Almost everything, stay tuned). I said, "Don't give me the bolus straight before the cathedar in my spine," He said, 'I've never done that before, I don't think it even works if I don't." But I had theorized that the bolus makes for too quick of a change for women and adds to the potential blood pressure drop. I said, "I don't want it!" He said, "how about I give you 25%?" I said, "okay." This turned out to be PERFECT. I could feel every wave still! Enough to breathe through each one. It even added to the possibility for the most redemptive part of this birth! (again, keep reading ;) ) |

Within an hour, the nurse said she'd like to check me because the baby had some decelerations. I agreed and we learned that I was 8cm open. I smiled. But the next wave came with something different. I said, "oh, this is much stronger." She checked again and baby's head was only one knuckle away from crowning! I said to Josh, "make sure you tell her what we want for the birth," And he started to describe how he was going to help receive the baby. The nurse said that isn't something they do there. And I said, "well we're probably just going to do what we want to do." Which we did :)
She walked out the room to call the doctor. I decided to see where I was at myself during a surge. I could feel the babies head too! Now my dreams were coming true. I kept checking to see if the baby would move past my pubic bone. And she did! I wasn't pushing AT ALL, just barely breathing her down. I said to Josh as I felt her stay put and low, "the baby is coming on the next one." He didn't even know I was doing what I was doing. He looked and said, "I don't even see a head." I said, "just wait, you will."
And there we were, receiving our baby, all by ourselves. This was a moment I'll never forget. Etched into a timeless place, we got exactly what we wanted. Josh supported my perineum (as he's been taught VERY well haha!). And he'd be proud to say, because of him, I didn't tear! I was SO happy because I wanted to birth on my hands and knees to prevent tearing, But because I was able to birth slowly and on my side, as well as with his help, it was all just fine. I said, "Josh, time?!" because I wanted to know what time just the head was born haha, he grabbed his phone and snapped a picture too and said, "1:55." The rest of her body was born at 1:56am on 11/5/2017 (about 49.5 hours after my water released) and she was right on my chest. "What is it?!" I exclaimed. And despite what 99% of people thought, he said, "It's a girl!"
And within about two minutes he said, "It's okay we'll try again." haha! I think he meant both for a homebirth and for a boy. But Lord knows, we're so far from controlling any of these things.
Thank you for reading! I'm sorry if I didn't mention your name if you were there as well. Know that I appreciate everyone so much and all of my homebirth team was perfect! It was me in the way, and this story is about just us :)
She walked out the room to call the doctor. I decided to see where I was at myself during a surge. I could feel the babies head too! Now my dreams were coming true. I kept checking to see if the baby would move past my pubic bone. And she did! I wasn't pushing AT ALL, just barely breathing her down. I said to Josh as I felt her stay put and low, "the baby is coming on the next one." He didn't even know I was doing what I was doing. He looked and said, "I don't even see a head." I said, "just wait, you will."
And there we were, receiving our baby, all by ourselves. This was a moment I'll never forget. Etched into a timeless place, we got exactly what we wanted. Josh supported my perineum (as he's been taught VERY well haha!). And he'd be proud to say, because of him, I didn't tear! I was SO happy because I wanted to birth on my hands and knees to prevent tearing, But because I was able to birth slowly and on my side, as well as with his help, it was all just fine. I said, "Josh, time?!" because I wanted to know what time just the head was born haha, he grabbed his phone and snapped a picture too and said, "1:55." The rest of her body was born at 1:56am on 11/5/2017 (about 49.5 hours after my water released) and she was right on my chest. "What is it?!" I exclaimed. And despite what 99% of people thought, he said, "It's a girl!"
And within about two minutes he said, "It's okay we'll try again." haha! I think he meant both for a homebirth and for a boy. But Lord knows, we're so far from controlling any of these things.
Thank you for reading! I'm sorry if I didn't mention your name if you were there as well. Know that I appreciate everyone so much and all of my homebirth team was perfect! It was me in the way, and this story is about just us :)
| Some people say I don't owe the world an explanation, but others say my honesty has encouraged and inspired them. I haven't shared my birth story yet, which I expected to be the most vulnerable story I would ever share. My breastfeeding story has turned out to be far more surprising. | Anaiah's birth was a planned home birth turned hospital transfer. I'll share this story another time. |
I knew from my breastfeeding experience with my older daughters that I wasn't one of the lucky ones with an abundance of milk; however, I assumed a lot about how much easier this would be given my education since my last baby. I got a jump start on supply and started doing things to avoid problems in the past even before I knew of any problem this time.
At first, I noticed Anaiah wouldn't latch at all on the left side. She saw our awesome chiropractor Dr.Chris Boman at day 3 and 5 of life and she began to take the left side. I figured this was the simple answer. Knowing my left side had a lot of catching up to do, I fed her as often as possible on that side. But she began to get frustrated there even though she would latch, and then she was frustrated at the right side as well. I thought my blistered nipples was from missing her top lip being rolled in. I was so exhausted the first few days of her life. After being up for practically three nights for her birth.
On day 5 of life I began to wonder why she wasn't peeing nearly as much as I thought she should. And I also wondered why my breasts, especially my left, seemed full but I couldn't express anything by hand or with a pump. I reluctantly decided to try a nipple shield and noticed she would latch on much easier. She seemed to need more stimulation at the roof of her mouth and this was giving it to her. This was my first disappointment as a lactation professional. I shouldn't have to use a nipple shield, how embarrassing. But she was sustaining sucks much longer so I thought it was best for the moment until I could find the energy and time to figure out more.
On day 6 my friend and fellow breastfeeding professional Ruthii Slatum came over to do a belly bind for me. This is when everything changed. She happened to be there when Anaiah peed a rusty color. I didn't know what this meant but Ruthii knew. She said it was dehydration. At this point I was already considering calling Kristen Davis, the local beloved IBCLC because of the lack of wet diapers and frustrating latch. Ruthii was gentle but frank about how much I was overlooking a problem from a breast augmentation I'd had four years prior.
I said, "but Ruthii, all our books and my teacher at UCSD said that as long as it's been a year and they're behind the muscle it's fine, right?!" Ruthii responded, "Karen, I'd encourage you to research that some more." My heart heard it but I was far from ready to accept this.
On day 5 of life I began to wonder why she wasn't peeing nearly as much as I thought she should. And I also wondered why my breasts, especially my left, seemed full but I couldn't express anything by hand or with a pump. I reluctantly decided to try a nipple shield and noticed she would latch on much easier. She seemed to need more stimulation at the roof of her mouth and this was giving it to her. This was my first disappointment as a lactation professional. I shouldn't have to use a nipple shield, how embarrassing. But she was sustaining sucks much longer so I thought it was best for the moment until I could find the energy and time to figure out more.
On day 6 my friend and fellow breastfeeding professional Ruthii Slatum came over to do a belly bind for me. This is when everything changed. She happened to be there when Anaiah peed a rusty color. I didn't know what this meant but Ruthii knew. She said it was dehydration. At this point I was already considering calling Kristen Davis, the local beloved IBCLC because of the lack of wet diapers and frustrating latch. Ruthii was gentle but frank about how much I was overlooking a problem from a breast augmentation I'd had four years prior.
I said, "but Ruthii, all our books and my teacher at UCSD said that as long as it's been a year and they're behind the muscle it's fine, right?!" Ruthii responded, "Karen, I'd encourage you to research that some more." My heart heard it but I was far from ready to accept this.
ANow very nervous for my baby's health, we called Kristen Davis and she came over in a heart beat. On her way over, I happened to check my facebook messages and one of my former students had offered me some extra expressed milk she had. I told her I'd probably need it and would get back to her soon.
Kristen spent hours with us! We tried three different pumps. I'd already borrowed two and Kristen let me borrow another type. We did a weight check and I learned that my daughter had dropped from her birth weight of 6lbs 11.5 oz to 5lbs 12oz. 13% And she was only transferring about 5ml at the breast!
Oh my God, I thought, I called my husband and asked him to go get that milk immediately. I was in complete shock. Kristen was so sweet and gentle and tried to take on my worry for me as much as possible, But I spent that night in panic and the next few nights on a roller coaster full of tears.
We started to investigate a posterior tongue tie. Kristen explained this so well. All the times I accused tongue ties and lip ties of being a trend was coming to bite me in the butt. Now I thought this was all I was dealing with ( as I was surely not ready to consider my surgery as a big problem at all yet).
Anaiah may very well have a posterior tongue tie and it could potentially improved her latch if we chose to revise it. However... the story continues to get more challenging then that.
Kristen spent hours with us! We tried three different pumps. I'd already borrowed two and Kristen let me borrow another type. We did a weight check and I learned that my daughter had dropped from her birth weight of 6lbs 11.5 oz to 5lbs 12oz. 13% And she was only transferring about 5ml at the breast!
Oh my God, I thought, I called my husband and asked him to go get that milk immediately. I was in complete shock. Kristen was so sweet and gentle and tried to take on my worry for me as much as possible, But I spent that night in panic and the next few nights on a roller coaster full of tears.
We started to investigate a posterior tongue tie. Kristen explained this so well. All the times I accused tongue ties and lip ties of being a trend was coming to bite me in the butt. Now I thought this was all I was dealing with ( as I was surely not ready to consider my surgery as a big problem at all yet).
Anaiah may very well have a posterior tongue tie and it could potentially improved her latch if we chose to revise it. However... the story continues to get more challenging then that.
I borrowed another pump from my generous fellow hypnobirthing educator. Lisa's daughter lent me one that seemed to be a bit better then the one I was already borrowing. I cried buckets over missing the bond of latching my daughter. I snapped this picture to remember how down I got.
The next week was full of pumping every two hours and celebrating every drop. I would still put my baby to breast every chance I got. Sometimes with the nipple shield sometimes without. One ml more then the day before, I still had hope. But my left side went from almost competing with my right to going back down to drops. The most I could pump was about 10ml from my right and 2 ml or so from my left.
Anaiah began to gain weight back quickly! And I had more offers for donor milk coming in. I tried to be thankful for the important things, but this was HARD. I wanted to breastfeed my daughter myself. Not just because it's embarrassing to struggle as a CLEC, but because I WANT TO FEED MY BABY! Why wasn't God yet answering my prayer the way I wanted? My heart was breaking into just as many pieces as when former traumatic things happened in my life. As I began to learn more about the kind of surgery I had and what that realistically meant, my heart broke more and more. I still believed and prayed for a miracle. And I still am!
I asked Kristen to come back to do another weighted feeding and help me with a hospital grade pump I finally got my hands on. I also wondered why pumping was hurting so bad and maybe I had the wrong size flanges.
I asked Kristen to come back to do another weighted feeding and help me with a hospital grade pump I finally got my hands on. I also wondered why pumping was hurting so bad and maybe I had the wrong size flanges.
5 different pumps, every supply supplement under the sun, and a diligence to try EVERYTHING.
When Kristen came back Anaiah was 12 days old and I'd been pumping religiously every 2-3 hours for the last 6 days straight as well as skin to skin and baby at the breast time as often as possible. This time, Kristen brought me different flanges and now I had the hospital grade pump so I still had hope. We'd also just ruled out the possibility of using domperidone because we did blood work and found that my prolactin levels were more than sufficient. Later I also got the results back from my midwife for progesterone levels and they were low, which ruled out retained placenta. It was starting to feel like the walls were closing in on me.
When I went to weigh Anaiah after a feeding at the breast, she was transferring the same as the first time we did this when she was totally weak and depleted. Her latch was better, but her suck was still not efficient. Probably because of a posterior tongue tie. But as I pumped and talked through things, the biggest monster came eye level with me and I couldn't ignore it anymore.
My nipples were restricted from scar tissue. My glands were restricted from expressing from scar tissue. Facing the reality that the choice I made when my life was completely different four years ago, it rocked me to my core.
I cried and moved through thoughts of failure, disappointment in myself, extreme regret. How could I face my husband? How could I face my daughter? How could I face myself? I made a decision that took away something from my family. How could I ever forgive myself for this. What does that mean for the future? We thought we'd have another baby, would that be completely irresponsible knowing I couldn't feed them my milk? Would I be able to get enough donor milk? How will I still help women after this kind of reality being who I am as an educator?
We prayed that night and I repented for this ignorant decision I'd made. We believed God, we still believe God could have mercy and change something about the structural damage I had. With my husband's encouragement, I decided to continue to pump more. But I was at the lowest of lows of hope.
When I went to weigh Anaiah after a feeding at the breast, she was transferring the same as the first time we did this when she was totally weak and depleted. Her latch was better, but her suck was still not efficient. Probably because of a posterior tongue tie. But as I pumped and talked through things, the biggest monster came eye level with me and I couldn't ignore it anymore.
My nipples were restricted from scar tissue. My glands were restricted from expressing from scar tissue. Facing the reality that the choice I made when my life was completely different four years ago, it rocked me to my core.
I cried and moved through thoughts of failure, disappointment in myself, extreme regret. How could I face my husband? How could I face my daughter? How could I face myself? I made a decision that took away something from my family. How could I ever forgive myself for this. What does that mean for the future? We thought we'd have another baby, would that be completely irresponsible knowing I couldn't feed them my milk? Would I be able to get enough donor milk? How will I still help women after this kind of reality being who I am as an educator?
We prayed that night and I repented for this ignorant decision I'd made. We believed God, we still believe God could have mercy and change something about the structural damage I had. With my husband's encouragement, I decided to continue to pump more. But I was at the lowest of lows of hope.
It's going to take me much much longer to process all of this. But I want to be thankful for what I have in the middle of such stress and sadness. Even with the new flanges and better pump, there's no improvement in supply or pain from pumping. It may actually be that pumping is furthering swelling in scar tissue. BUT! My daughter will still take my breast! I don't think she's transferring anything significant, but what a miracle she hasn't rejected me at least not yet. I asked myself, how long do I wait for a miracle, how do I know what God's answer is for my prayer?
Well of course, as the mystery of life would have it, I named my daughter "Anaiah" which actually means "God answers"
I don't know what's going to happen. I know I'm going to have to ask for donor milk now for the foreseeable future. I know my daughter needs me for more than just milk. And my husband has reminded me to be proud of myself and that " I didn't marry you so you could breastfeed." Funny how I actually attributed my identity as a wife and mother to that ability more than I ever knew.
I've learned that breastfeeding far outweighed my desire for a home birth. It far outweighed my desire for most things.
Thank you so much for all the prayers and believing with me. Thank you so much for the encouragement and still accepting me as someone who wants to help others, even if I struggle myself.
I appreciate all of the suggestions and I know many of you will still have suggestions and maybe even have an opinion on how I should do things differently. Please just be careful of my heart as I put myself out there so publically about all of this. I am taking the risk of exposing myself greatly and at the cost of something that makes me more vulnerable then I ever knew. I can only hope that my story, whether successful the way I want or not, still promotes hope and faith for someone out there.
Thank you SO MUCH to Ruthii, Kristen, Chris, and the donor moms. You've saved my daughter's life. If it wasn't for you all, she surely would be in the NICU!
Temecula HypnoBirthing and | Welcome Lisa! Today I met again with Lisa Skeels, to discuss how we can join forces to meet more families in more areas! Lisa is another HypnoBirthing instructor who generally serves the Riverside area, as well as other areas more north of there. And she also takes doula clients in the Temecula area as well, I'm so thankful that we've come up with a way to spread the word on what HypnoBirthing is in these areas now as a force! I'm also excited that I have someone to fill in for me during the months I'll be on Maternity leave. And I will still fill in for her now and then if necessary as she is still attending births as a birth doula. This is a really great partnership for us, and a really great opportunity for parents to be able to have access to more options, in more places, more often! |
HypnoBirthing is just a method, not a standard of birthing any kind of "right" way. The last birth I attended was a great example of how natural birth can look very different than the movies we watch in class, yet just as triumphant!

I met Deena in the first unit of HypnoBirthing for her childbirth class I taught. It was really amazing how obviously instinctual she was and how obviously protective her husband Jason was. It was funny because he didn't even know anything about my class until she said she was going that day.
They asked me to be their Doula after her classes were over. At first I was reluctant because she was choosing to birth at Rancho Springs. It is a hospital that does not have the reputation for supporting evidence based birth. I've seen more than my fair share of coercion and manipulation in labor and delivery rooms. I really prefer to make it next to impossible to ever witness more. Not every doula feels that way, but that's were I'm at currently. Nevertheless, being that we'd already had a relationship as teacher and student, and that I knew she was a strong woman - I accepted the honorable invitation to be there.
I accepted the fact that even though she really wanted a home birth, but it was just not in the cards this time. We talked at length about how to advocate for the kind of physiological experience she wanted. I went to one doctors appointment with her when she was 40 weeks. She brought an article about delayed cord clamping and her birth plan. I witnessed her going through her birth plan with her doctor. Then I got into a cordial dialogue about optimal cord clamping as the doctor invited my opinions, I was slightly more optimistic about the OB after this exchange. Deena wasn't so hopeful. I wanted to stay open and I hoped that her OB would continue this open dialogue for more compromise. However, she did at one point say to Deena after trying to debate the evidence for leaving a cord in tact until it's done pulsating, "you know you're not the captain of this ship. If anything, you might be an officer, but you have to trust me." Deena and I shook our heads later at how unethical that statement was. I think it solidified Deena's fears that her doctor wasn't really going to honor her Hippocratic oath to provide Deena with informed consent and refusal. It felt like she was insinuating that regardless of evidence, she would be the one making the final decisions.
The doctor did invite me to send her an email about evidence for in tact cords. I did so the next day and also asked her to lunch or coffee. I followed up to make sure she got the email too. Yet never any response was received unfortunately.
On 1/21 when Deena was 41 weeks and 4 days pregnant, I got a text from that her upper back was hurting. I stopped by quickly to give her some China gel for her back and to talk to her baby girl. I put my head and my hands on her belly and I asked Emery, "hey what are planning on for today?" I felt like Emery said she was just going to hang out with her mom. So I said "Emery! You can hang out with your mom out here! Do you want to do girly things together? You can get your hair done and your nails... and her mom added, "and shopping!" We encouraged Emery to come out and go to Target with us.
On 1/22 I got a text from Deena at 5am that said "call me when you wake up, I think I'm in labor." I called her immediately and she answered asking, "what are you doing up so early?" I responded humorously, "why are you in labor so early?" She laughed. It was the beginning of the biggest storm this city has seen in a long time. And it was the beginning of her birth.
She said she'd been having far apart surges (contractions) since 11pm and she'd slept maybe an hour or two. I reminded her the importance of sleep and asked her to please make an effort to sleep more. As the story unfolds you'll learn that her decision not to sleep may have been why her birth was so long, but her stubbornness would transfer perfectly into perseverance.
I stayed in touch a couple times throughout the day. She still wasn't sleeping so I just waited for her to tell me it was time for me to come.
I Arrived at 2:15pm on 1/22 but It was relatively evident that sleep was still a real need. So I tucked her back into bed and left at 3:30pm. She seemed to have at least a decent short nap.
That night I was asked to come back again and I arrived at 1:04am on 1/23. Rocko the dog was wearing a bow-tie. Grandma was so helpful and a calming presence for everyone.
By 1:58 I recorded that there were still consistent surges since I got there. It was looking more active now. Lots of vocalization. Birth show (bloody show) was visible, but she's very vascular, so that's been going on as expected. It did seem much more active than before.
She drank water after every surge. She ate a banana.
Her mom, my favorite Grandma of all time for births was making jokes about using the heat pack herself at 2:20am.
Deena finished eating a peanut butter and honey toast at 2:53am , she didn't really like eating the last bite. She became a little bit shaky a while before, but deep breaths rid her of the shaking. I was so proud of her for eating and I called her my "best eater yet." Jason jokingly added, "yeah she is." Which gave grandma and I a good laugh.
She continued drinking water after every surge so diligently and she used the restroom periodically.
4am she tried the shower.
4:15 out of the shower.
Then she was trying to sleep and side lying, but surges started getting more close (guessing 3-5 mins).
At 5:25am she got in the bath feeling very worn out.
We hoped the bath will either slow it down enough to get better naps, or relax her muscles enough to get her body to open faster.
She said the bath made it feel much less intense and she started dozing off in-between her waves.. Thank goodness. Surges spaced from 4 to 5 mins apart. Some closer, but now lasting only 30 seconds instead of 60-90. At 7am she was thinking maybe her water released in tub - but it didn't. She got out of bath. Surges were much stronger now.
Deena asked her mom for a cutie (orange) Jason responds, "you got one right here."
We put her hair up and dad lint brushed her dress as I mentioned "you have to be sexy to give birth." Jason added, "always sexy for my baby momma"
Despite the hopefulness that one nap would do something, I could tell she was still getting worn out. So now it came down to either trying to make baby come out faster or back to the bath for more rest. She described her energy as still there so we tried Deep squats and acupressure. But she was really loosing steam around 8:15am.
| This would probably be the point where most women would throw in the towel. Not Deena. So I called a midwife friend to see what the chances were that she could come check on Deena so we could get some more information. She said she could! Thank goodness! Cristi came to check at 9:35am. Baby sounded great and now we learned what her cervix was doing. She was 3cm open, 100% thinned out, fully anterior cervix, baby was -2 station. Baby seemed Perfectly positioned, and she had a bulging bag of water. Cristi was so encouraging, but she did mention sleeping with an epidural since it was obvious rest was the highest priority to everyone. Deena immediately shook her head to sign "no". Wow, I thought. She is so impressive! | Cristi left and now that we knew it was truly proven that rest was number one, back in the bath Deena went at 10am. She was able to get some rest so I left to clean myself up and hopefully rest a bit too. I never rest well at births like this, it so hard to leave my strong mommas and not wonder if their okay every minute I'm gone. But I was able to sleep an hour. Before I'd left, I asked our amazing chiropractor Chris Boman to come help her out. He was kind enough to agree to come on his lunch. And in hopes he could do something magical, I came back at 1:30pm. Between the time I left and came back, Cristi had offered to support a home birth for them. I communicated that to Grandma and hoped that Deena and Jason would consider it. But I was shocked to find out, they agreed to do it! They decided to hire a midwife while in labor. What a satisfying triumph to witness! |
Dr.Chris had just adjusted her when I arrived. She went back in the tub again. She said she's visualizing opening up even while resting in the tub. She's was confident it blows my mind. At 3:05pm She said she was so happy she doesn't have to leave home anymore. That no one is going to threaten the bonding moments she gets after birth. I told her, "yes, you're worth it!" She corrected, "no, she's worth it," and rubbed her belly. My eyes watered and I affirmed her already incredible mothering abilities. It seemed like now she could open up in the comfort of her safe place.
I began to time some Surges to show to Cristi. They were now 6 1/2 mins apart. Lasting 90 seconds. So good rest could still be had, but when they came - they were strong and hopefully effective. Cristi was on her way back over.
Cristi arrived at 3:11pm. She brought the birthing tub. Soon the wonderful team would show up as well. We had a second midwife named Amy and a student midwife named Rachel. All totally genuine, skilled, kind, prepared and good providers. Jason went to the store to get a tarp and an air pump. Cristi set up all her things as I stayed with Deena still in her bath. Deena ate oranges and a honey stick. Her mom made some amazing chicken soup too.
Deena felt some rectal pressure 3:25 and I was exited. At 3:43 she said, "Maybe my birth is so long because I'm supposed to inspire other women that they can do it too." I appreciated that, but reminded her that she doesn't have to perform for anyone!
At 4:39 the birth tub (which looked more like a pool) was being filled up. I worried I was going to have to cancel my class that night because she seemed complete. Her back up doula was ready but it was a very tricky time!
At 4:55pm Cristi said she's 7cm -1 station. Even though she wasn't complete, it really seemed like she was going to have this baby soon since she described more and more pressure. So I texted to tell my students I would be staying.
Sure enough, at 6:15pm Cristi checked again and she was about a -1/0 station and she only had a tiny anterior lip of cervix left. I was so glad I postponed my class. The next few hours were a combination of trying to push with no natural expulsive reflux (fetal ejection reflux) and resting to do more of a labor down thing. It was obvious that Deena's uterus had little to no energy left help her with pushing. Grandma put snacks out for everyone, Jason ordered pizza, and I asked my husband to bring us a pot of coffee.
I stayed in the bath with her and things were really pretty rough. I regretted not helping her use more of her HypnoBirthing tools to get her in a deeper state sooner. We had her crowning rose picture on the wall and she listed to Deep Theta the whole time, but I really wanted to take her to a better inner-focused place. Everyone left the room for a moment, and I decided what a perfect time to try. I talked her through relaxation and the next surge she had was completely relaxed. I was so glad for her. But then either because we just didn't have enough time or she was getting distracted from people coming back in the room, her surges grew back to taking her over.
At 9:15 pm our hero of a Chiropractor Dr. chris came back and adjusted Deena and then the rest of the team too! He joked he was onto us, the real reason we ask him to come to births for our own adjustments.
Cristi suggested Deena lie down with Jason and try to sleep. We all hoped that one more nap would get her some kind of natural expulsive reflux so she wouldn't have to be doing all the work herself to push. Alas, we were wrong about the sleep option. That adjustment and getting out of the water was just what her body needed to pick up in consistency of waves.
I began to time some Surges to show to Cristi. They were now 6 1/2 mins apart. Lasting 90 seconds. So good rest could still be had, but when they came - they were strong and hopefully effective. Cristi was on her way back over.
Cristi arrived at 3:11pm. She brought the birthing tub. Soon the wonderful team would show up as well. We had a second midwife named Amy and a student midwife named Rachel. All totally genuine, skilled, kind, prepared and good providers. Jason went to the store to get a tarp and an air pump. Cristi set up all her things as I stayed with Deena still in her bath. Deena ate oranges and a honey stick. Her mom made some amazing chicken soup too.
Deena felt some rectal pressure 3:25 and I was exited. At 3:43 she said, "Maybe my birth is so long because I'm supposed to inspire other women that they can do it too." I appreciated that, but reminded her that she doesn't have to perform for anyone!
At 4:39 the birth tub (which looked more like a pool) was being filled up. I worried I was going to have to cancel my class that night because she seemed complete. Her back up doula was ready but it was a very tricky time!
At 4:55pm Cristi said she's 7cm -1 station. Even though she wasn't complete, it really seemed like she was going to have this baby soon since she described more and more pressure. So I texted to tell my students I would be staying.
Sure enough, at 6:15pm Cristi checked again and she was about a -1/0 station and she only had a tiny anterior lip of cervix left. I was so glad I postponed my class. The next few hours were a combination of trying to push with no natural expulsive reflux (fetal ejection reflux) and resting to do more of a labor down thing. It was obvious that Deena's uterus had little to no energy left help her with pushing. Grandma put snacks out for everyone, Jason ordered pizza, and I asked my husband to bring us a pot of coffee.
I stayed in the bath with her and things were really pretty rough. I regretted not helping her use more of her HypnoBirthing tools to get her in a deeper state sooner. We had her crowning rose picture on the wall and she listed to Deep Theta the whole time, but I really wanted to take her to a better inner-focused place. Everyone left the room for a moment, and I decided what a perfect time to try. I talked her through relaxation and the next surge she had was completely relaxed. I was so glad for her. But then either because we just didn't have enough time or she was getting distracted from people coming back in the room, her surges grew back to taking her over.
At 9:15 pm our hero of a Chiropractor Dr. chris came back and adjusted Deena and then the rest of the team too! He joked he was onto us, the real reason we ask him to come to births for our own adjustments.
Cristi suggested Deena lie down with Jason and try to sleep. We all hoped that one more nap would get her some kind of natural expulsive reflux so she wouldn't have to be doing all the work herself to push. Alas, we were wrong about the sleep option. That adjustment and getting out of the water was just what her body needed to pick up in consistency of waves.

I'm reluctant to say this being that I teach a method of childbirth that promotes the possibilities of comfortable natural birth. But, Deena's next handful of surges were probably full of the most expression of discomfort I've ever seen. And this was my 79th birth. If it was hard to watch for me, I can't imagine how it was for Jason and her mom as well. All of us just wanted to relieve her!
At 9:20pm the pizza man came while Deena had a crazy strong surge. Deena was in her room with Jason and I. Deena was LOUD. I mean, the neighbors down the street could have heard her if the window was open. It was the kind of National Geographic, wild animal, crazy thing you hope to avoid in HypnoBirthing. Her body was flaying around. She was groaning with a sort of projection you wouldn't imagine possible in a beautiful feminine woman like herself. The pizza man might have decided not to do deliveries anymore. He arrived hearing all of that and seeing a bunch of women dressed like nurses and a Chiropractor with a table in the living room. Poor pizza man.
Anyways, it was time to help Deena more.
At 9:51 the midwives asked to release her water and Deena agreed. We then moved her onto pushing on the birth stool.
Deena WORKED. Never once did she really get a good reflux. She had to do all of the work to push, and we're talking about at hour 4 of being completely open. Yikes. We all coached her to keep going, keep going, keep going. She would never give up but it was HARD. She almost said, "I can't," but Jason interrupted her and said "don't start." She needed that. It was strong but came with love and trust in her abilities.
Baby was at a plus three station at 11pm . How I ironic I thought, were only one hour from the 24th, which is the anniversary of something very special to this family. Deena was only one hour from being 41 weeks and 6 days pregnant, the day her induction was scheduled.
Yet, at exactly 11:24pm (there's that 24), Baby Emery arrived with a lot of surprise! After all of that, the last push some how shot her out like a rocket. Her legs flew towards the floor as Cristi gripped her head and shoulders. All of our eyes widened and watered as we listened to Deena speak to her daughter in her arms for the first time.
She said "it's okay it's okay" and "Hi baby" "Hi Emery."
Emery was so cute and perfect! She only took a short while to work out some fluid, and her cord stayed in tact the whole first hour to get her the extra oxygen she needed.
Deena's uterus was pretty much done doing anything. So her bleeding was on the side of too much. A shot of pitocin in the thigh, would be in good order.
The Cord was clamped and cut by the new Daddy at 12:20 am.
So much for the debate Dr.UnEthical!
The Placenta was birthed at about 12:30am, I held Deena up to squat on the bed to push it out. Baby Emery latched approximately at 12:34am. Much to my surprise she did pretty instinctually after such a journey for her.
The new parents cuddled each other in their own bed. Completely in charge of their family. After a birth that was beyond challenging, I couldn't think of a better reward. The midwives noticed the coning on Emery's head was slightly crooked. Now it made sense why the Chiropractor helped so much. Whatever was going on internally was keeping Emery from perfectly lining up. Not enough to make it impossible of course, but probably a piece of the challenge.
Emery weighed 8lbs and 10oz. She was 21inches long. She looks JUST like her Daddy. And now it's clear to me that she's not just going to like shopping with her mom, she's also going to LOVE being spoiled yet taught to be strong by her Daddy.
Emery, Deena, and Jason, you told me months ago that your family legacy was being a hard working family. Now it's clear why. The three of you will NEVER give up on each other. God bless you with fruitfulness for all of your perseverance! And thank you for allowing me to be there with you for your warrior birth.
At 9:20pm the pizza man came while Deena had a crazy strong surge. Deena was in her room with Jason and I. Deena was LOUD. I mean, the neighbors down the street could have heard her if the window was open. It was the kind of National Geographic, wild animal, crazy thing you hope to avoid in HypnoBirthing. Her body was flaying around. She was groaning with a sort of projection you wouldn't imagine possible in a beautiful feminine woman like herself. The pizza man might have decided not to do deliveries anymore. He arrived hearing all of that and seeing a bunch of women dressed like nurses and a Chiropractor with a table in the living room. Poor pizza man.
Anyways, it was time to help Deena more.
At 9:51 the midwives asked to release her water and Deena agreed. We then moved her onto pushing on the birth stool.
Deena WORKED. Never once did she really get a good reflux. She had to do all of the work to push, and we're talking about at hour 4 of being completely open. Yikes. We all coached her to keep going, keep going, keep going. She would never give up but it was HARD. She almost said, "I can't," but Jason interrupted her and said "don't start." She needed that. It was strong but came with love and trust in her abilities.
Baby was at a plus three station at 11pm . How I ironic I thought, were only one hour from the 24th, which is the anniversary of something very special to this family. Deena was only one hour from being 41 weeks and 6 days pregnant, the day her induction was scheduled.
Yet, at exactly 11:24pm (there's that 24), Baby Emery arrived with a lot of surprise! After all of that, the last push some how shot her out like a rocket. Her legs flew towards the floor as Cristi gripped her head and shoulders. All of our eyes widened and watered as we listened to Deena speak to her daughter in her arms for the first time.
She said "it's okay it's okay" and "Hi baby" "Hi Emery."
Emery was so cute and perfect! She only took a short while to work out some fluid, and her cord stayed in tact the whole first hour to get her the extra oxygen she needed.
Deena's uterus was pretty much done doing anything. So her bleeding was on the side of too much. A shot of pitocin in the thigh, would be in good order.
The Cord was clamped and cut by the new Daddy at 12:20 am.
So much for the debate Dr.UnEthical!
The Placenta was birthed at about 12:30am, I held Deena up to squat on the bed to push it out. Baby Emery latched approximately at 12:34am. Much to my surprise she did pretty instinctually after such a journey for her.
The new parents cuddled each other in their own bed. Completely in charge of their family. After a birth that was beyond challenging, I couldn't think of a better reward. The midwives noticed the coning on Emery's head was slightly crooked. Now it made sense why the Chiropractor helped so much. Whatever was going on internally was keeping Emery from perfectly lining up. Not enough to make it impossible of course, but probably a piece of the challenge.
Emery weighed 8lbs and 10oz. She was 21inches long. She looks JUST like her Daddy. And now it's clear to me that she's not just going to like shopping with her mom, she's also going to LOVE being spoiled yet taught to be strong by her Daddy.
Emery, Deena, and Jason, you told me months ago that your family legacy was being a hard working family. Now it's clear why. The three of you will NEVER give up on each other. God bless you with fruitfulness for all of your perseverance! And thank you for allowing me to be there with you for your warrior birth.
Yes, I said that about UCSD ditching their Hillcrest location for births. I realize I'm part of a small portion of spoiled rotten birth nerds. I just had to go on the tour to make sure that I could ease up on my anxiety so I wouldn't bring that into the birth space of any parent. I LOVED the Hillcrest location and I realize the midwives are the same. But the culture of a true midwifery model of care within a hospital is so unique that it's hard to believe it could transfer anywhere so easily.
| I toured with two other doulas and one of my HypnoBirthing students. In case you're wondering, why is a doula from Temecula writing about a hospital in San Diego and why does she care this much? It's because the options for birth here in the natural birthing community (or even the evidence based and educated community) are non existant unless you can have an out of hospital birth. |
Here are some pictures that say it all when it comes to the "modern" style of this place!
If you're HypnoBirthing, you should be arriving with an eye mask on and head phones in anyways. So I suppose none of this really matters. And I realize there are plenty of people who think this is pretty.
So let's get practical..
What you really want to know is are things going to be practically different here.
PARKING & DIRECTIONS
Don't go to the Thorton entrance! Go around the building across from the emergency room. 8am-4:30pm there is Valle parking at the Thorton enterance if you should go there; however, you're making mom walk a lot further. Both enterances are open 24hrs a day 7 days a week,
There are no street parking options. You must park in a paid space and it's $8 per 24hr period. You can still drop off mom in labor at the pull up enterance and there you'll find the big wheel chairs if mom prefers. The Birth Center, the traditional Labor and Delivery, and the OR are all on the 9th floor. The postpartum rooms are on the 10th floor. The NICU is on the 8th floor. All moms get triaged before entering either the Birth Center rooms or the Labor and delivery rooms. Triage rooms are prepared for deliveries should the birth go too quickly. The triage rooms and Birth center are to the left, the Labor and Delivery are to the right. To see videos on the proper enterances and the halls you walk through, see my facebook! www.facebook.com/temeculahypnobirthing
PARKING & DIRECTIONS
Don't go to the Thorton entrance! Go around the building across from the emergency room. 8am-4:30pm there is Valle parking at the Thorton enterance if you should go there; however, you're making mom walk a lot further. Both enterances are open 24hrs a day 7 days a week,
There are no street parking options. You must park in a paid space and it's $8 per 24hr period. You can still drop off mom in labor at the pull up enterance and there you'll find the big wheel chairs if mom prefers. The Birth Center, the traditional Labor and Delivery, and the OR are all on the 9th floor. The postpartum rooms are on the 10th floor. The NICU is on the 8th floor. All moms get triaged before entering either the Birth Center rooms or the Labor and delivery rooms. Triage rooms are prepared for deliveries should the birth go too quickly. The triage rooms and Birth center are to the left, the Labor and Delivery are to the right. To see videos on the proper enterances and the halls you walk through, see my facebook! www.facebook.com/temeculahypnobirthing
| There are gaurds when you walk past this sign to the left. They are there until 11:30pm (but they're working on getting 24-hr guards). If they're not there, just press the button on the black box and the nurses will buz you in the door after speaking with you through the speaker. | This is one of the waiting rooms areas right there past the gaurds. |
FOOD?
One of the Dads on the tour asked how to get deliveries while here. GREAT question guy! You can meet them on floor one in the loby in case anyone else it that smart. Otherwise, there is a cafeteria on the bottom floor and it closes at 8pm. There are vending machines around as well. There is not a place the doula can go in and get water and snacks for the mom or family, which isn't different than UCSD. We still need to ask the nurses for those things. Food for the patient is delivered to the room unless mom has an epidrural, but not for the other parent.
One of the Dads on the tour asked how to get deliveries while here. GREAT question guy! You can meet them on floor one in the loby in case anyone else it that smart. Otherwise, there is a cafeteria on the bottom floor and it closes at 8pm. There are vending machines around as well. There is not a place the doula can go in and get water and snacks for the mom or family, which isn't different than UCSD. We still need to ask the nurses for those things. Food for the patient is delivered to the room unless mom has an epidrural, but not for the other parent.
STUFF
The big red bean bag is still with us! Hurray! The labor and delivery rooms do not have any squat bars yet, but they have been ordered. There are birth balls and peanut balls. IBCLCs are available during the working hours 7 days a week. Kids are allowed everywhere (including any birthing rooms) unless there's an outbreak of the flu or anything similar and they're not allowed to stay over night. There is only ONE refridgerator and it's in my favorite waiting room.
One of the best things:
Labor and delivery had WIRELESS MONITORS! They are the kind with the little pack you carry around, but you can still get in the shower with them as long as the power pack isn't getting wet. (THIS IS A FANTASTIC THING COMPARED TO OTHER HOSPITALS in case you didn't know!) As far as monitoring in the Birth Center, it's still with a doppler periodically as usual.
The big red bean bag is still with us! Hurray! The labor and delivery rooms do not have any squat bars yet, but they have been ordered. There are birth balls and peanut balls. IBCLCs are available during the working hours 7 days a week. Kids are allowed everywhere (including any birthing rooms) unless there's an outbreak of the flu or anything similar and they're not allowed to stay over night. There is only ONE refridgerator and it's in my favorite waiting room.
One of the best things:
Labor and delivery had WIRELESS MONITORS! They are the kind with the little pack you carry around, but you can still get in the shower with them as long as the power pack isn't getting wet. (THIS IS A FANTASTIC THING COMPARED TO OTHER HOSPITALS in case you didn't know!) As far as monitoring in the Birth Center, it's still with a doppler periodically as usual.
HOW MANY OF THINGS?
There are 3 Birth Center rooms, 8 Labor and Delivery Rooms, and 3 OR rooms. The recovery time spent in the OR area for a Belly Birth, before going to postpartum is 1-2 hours. The same goes for vaginal deliveries in either room. I have to be honest, I'm worried about the number of Birth Center rooms and how close they are to the Labor and Delivery. Is there any way the nurses and midwives can remain unbiased about helping women maintain their goals in staying in the birth center? Or would they just keep their birth plans supported in the Labor and Delivery rooms (like they did for various reasons in Hillcrest). Being in a room where the epidural is readily available is obviously going to make a difference in my opinion. Sometimes, in Hillcrest, it was the simple fact that changing floors was too much of a hastle and moms would stick to their natural birthing goals.
OTHER NOTES
Twins still push in the OR (like most hospitals), the midwives aren't "officially" delivering breech (although we all know they have in the past) and if you're looking for a doctor who is experienced in breech vaginal birth, Dr.Herbert (the doctor there most of the time) is known to have that skill.
There are 3 Birth Center rooms, 8 Labor and Delivery Rooms, and 3 OR rooms. The recovery time spent in the OR area for a Belly Birth, before going to postpartum is 1-2 hours. The same goes for vaginal deliveries in either room. I have to be honest, I'm worried about the number of Birth Center rooms and how close they are to the Labor and Delivery. Is there any way the nurses and midwives can remain unbiased about helping women maintain their goals in staying in the birth center? Or would they just keep their birth plans supported in the Labor and Delivery rooms (like they did for various reasons in Hillcrest). Being in a room where the epidural is readily available is obviously going to make a difference in my opinion. Sometimes, in Hillcrest, it was the simple fact that changing floors was too much of a hastle and moms would stick to their natural birthing goals.
OTHER NOTES
Twins still push in the OR (like most hospitals), the midwives aren't "officially" delivering breech (although we all know they have in the past) and if you're looking for a doctor who is experienced in breech vaginal birth, Dr.Herbert (the doctor there most of the time) is known to have that skill.
Birth Center pics!
Labor and Delivery room pics
Just breathe...
It's going to be okay! This is still a wonderful place to birth. The midwives will not fail us through this transition. I have always been completely impressed with their skills and true respect for the physiological process. Just continue to keep that Belly Birth rate low and listen to educated mommies who deserve respect UCSD, and we'll keep on lovin' ya!
I can't begin to describe how excited I am about this new birth center! The midwives who are opening it and providing excellent care there are Karen Pecora and Cristi Lewis. They are already loved and adored midwives who will continue to provide care for home birthers, while offering this birth center option for others. They will be offering care for VBACs, they do accept Medi Cal, and they will have tubs for water birth!
How great is that?!
How great is that?!
| Additionally, they have space in their center for classes and I'm honored to say that I have been invited to teach HypnoBirthing there! My first fall brook session will begin November 5th and continue for 4 more consecutive Saturdays. It will be from 2pm-5pm. Hopefully this will be a good option for both the North County San Diego families as well as the Temecula Valley families. Stay tuned for more information about this awesome opportunity for education as well as peaceful, safe, beautiful birth! |
If you read my last two blogs, you know that OBGYNs and Midwives are both medical professionals that provide care for birthing women. They practice differently, not just because of money; rather, a cultural perspective of birth that's practically opposite. We do have some Doctors that we love and are within reach from our little Valley in the Temecula area. We also have different kinds of midwives that provide different options and potential for charging your insurance company. So now, it's time to talk Doulas. First, here's some pictures of myself - in action - as a birth doula.
As you can see, I don't really have that many pictures of myself doing something at the birth. Most of these are after the birth or at the postpartum visit. Usually, I'm very focused on what's happening with the mom. If there's a chance for a picture, it's because I'm grabbing a camera to capture the beautiful connection between Mom and Dad. Out of 73 births, I've only had two where there was a photographer. So that's where those pictures came from. You can see that my face is often pretty close to the mom's especially in times where she needs to hear encouraging words. I use words a lot because of my HypnoBirthing training. Our words are so powerful. One time I led an unmedicated laboring woman to sleep with relaxing words in-between surges (contractions) at 9 cm. Sometimes, however, it's the exact opposite. Sometimes I'm massaging her feet and saying nothing. Sometimes, what she needs is to be all alone and I'm just setting up the room for when she gets out of the bathroom. My role can vary so much! One time I was blow drying my client's hair, many times I've taken parents on walks outside, Often I'm helping the Dad communicate with the hospital staff or finding creative ways to communicate the parent's desires without actually speaking them to the nurse or doctor. Because of my lactation certification, I usually help the nurses out by getting things started with breastfeeding.
First, let's talk about what a doula is NOT.
One thing a doula is NOT, is a medical professional. They do not take fetal heart tones (although many times I find myself trying to help the nurse get the baby's heart rate if she is struggling to get her work done and the mom is moving around a lot). They do not do vaginal exams generally speaking (although some doulas are also student midwives or former labor and deliver nurses and do include that). They do not deliver the baby or perform clinical tasks, although they might be the most qualified person to help someone in a situation where there is an accidental car birth or something of the sort. If you read the previous blogs you know that OBGYNs and midwives are medical professionals, so to set the record completely straight: A doula is not the same thing as a midwife.
So how does a doula get their education?
Some doulas are not officially trained or certified at all. Sometimes they just fall into the role because they have 6 friends who all asked them to be at their side while they birthed. But for most very active birth doulas, they do seek formal education and usually some kind of certification. There are different programs that certify and educate doulas. The most popular is DONA. But there's also CAPPA, ToLabour, and probably a few others out there. The trainings consist of a weekend course. Sometimes 3 or 4 days. The certification process is much greater. I am certified with DONA. This required reading a variation of books about birth and being a support person at a birth as well as breastfeeding, attending births and being evaluated by the medical professionals, continuing education (like my acupressure certification), and writing essays and taking tests. All that work couldn't possibly compare to the hands-on education I've received simply from attending all kinds of births.
| * Side note: Here's some ironic perspective, an EMT is qualified to deliver a baby, but has no hands on experience witnessing live births. A paramedic is only required to spend three shifts in labor and delivery where they usually don't get to do anything but watch and all of the births are hospital births, which means it's highly unlikely they're witnessing a birth that would compare at all to what they would see in the field. This is a picture of me following the ambulance carrying my client after an accidental homebirth. The paramedic attending was extremely nervous and visibly shaking, I was calming down the emergency personal there. Birth can truly only be something you're comfortable with after witnessing it so many times. |
So what does a doula actually do?
| A doula is there to help the parents have the birth they envision. Whatever that may be. Sometimes that's not a natural birth! But usually parents hire a doula with the intention of at least trying for a natural birth. Doulas do not want everyone to have a certain kind of birth, they want the parents to be able to look back and be able to say. "we know we did everything we could to have the birth we wanted because of your support." Doulas understand the extreme impact of your birth experience and take into careful consideration how it can make an impact on your postpartum emotional status. 15%-20% is what our country is looking at for postpartum depression, and that's only the reported cases! Birth Doulas do not want your birth experience to seem like it got high-jacked, they want you to know what you need to surrender to vs. what is really in your control. Some people say a birth doula is like a wedding planner, but for the birth instead. |
But wait, there's more!
Just because a doula is not a medical professional doesn't mean the don't know how to help you have a safe experience. Having a doula takes away the pressure from the Dad to have to remember every little thing he learned in your childbirth education class. What are the signs of infection? What are signs of progress? What are all the different positions we can try? What do I need to say to her to help her release fear and ease into a more efficient birth? What was that drug their suggesting all about again? A doula will make sure that you get informed consent, that you know all the benefits and risks of every single turn of events. If a nurse is making a suggestion, the parents can ask for a moment to discuss it, and your doula will remind you not only all of the benefits and risks, but also the alternatives to that intervention.
Doulas definitely maintain the midwife philosophy which is that you don't fix what's not broken and physiological birth works left alone in the body of a confident woman who feels safe and comfortable.
Some doulas are real google experts. Just kidding, it's not the doctor-google sort of thing. But doulas will have a real medical journal or scientific study for you to check out on a dime, just to make sure you can feel confident about whatever decision you're making. For example, I've read EVERY SINGLE SCIENTIFIC STUDY ON GBS THAT EXSISTS. Yeah, that took a while!
Doulas definitely maintain the midwife philosophy which is that you don't fix what's not broken and physiological birth works left alone in the body of a confident woman who feels safe and comfortable.
Some doulas are real google experts. Just kidding, it's not the doctor-google sort of thing. But doulas will have a real medical journal or scientific study for you to check out on a dime, just to make sure you can feel confident about whatever decision you're making. For example, I've read EVERY SINGLE SCIENTIFIC STUDY ON GBS THAT EXSISTS. Yeah, that took a while!
Different shapes and sizes...
Some doulas do this and some doulas do that. Some doulas are also childbirth educators, like myself, and some doulas maintain different philosophies within those different methods of natural birth education. I've taken nearly every method of childbirth education there is, and picked up different tricks from all of them. But I definitely maintain a priority in the mental and emotional components, especially a lack of fear.
Some doulas are placenta encapsulators, I am not. Some have worked with a lot of military families. Some, like myself, know what it's like to birth without a husband for reasons beyond a deployment.
Some doulas work in groups, some work in partnerships. Unless you say otherwise, all doulas will have a back up doula for your birth in case of emergency.
Some doulas specialize in multiples (twins and triplets), some specialize in VBACs, some are more experienced with home birth, and some are very particular in which hospital they will or won't work within. Unfortunately, I've witnessed more coercion that I can stomach, so I'm very limited now in what clients I'll take. I expect my clients to go out of their way to truly make sure they're in the best hands they can possibly be in.
Some are also postpartum doulas, some have lactation certifications (I'm a CLEC). Some are also massage therapists, and some are even Labor and Delivery Nurses too, Some are professional photographers!
We usually say that you should interview about 3 doulas and really go with your gut on who is going to make you and your support team feel the most comfortable.
Generally speaking, they all normally do at least one or two prenatal visits, attend the birth for it's entirety, and one postpartum visit.
Some doulas are placenta encapsulators, I am not. Some have worked with a lot of military families. Some, like myself, know what it's like to birth without a husband for reasons beyond a deployment.
Some doulas work in groups, some work in partnerships. Unless you say otherwise, all doulas will have a back up doula for your birth in case of emergency.
Some doulas specialize in multiples (twins and triplets), some specialize in VBACs, some are more experienced with home birth, and some are very particular in which hospital they will or won't work within. Unfortunately, I've witnessed more coercion that I can stomach, so I'm very limited now in what clients I'll take. I expect my clients to go out of their way to truly make sure they're in the best hands they can possibly be in.
Some are also postpartum doulas, some have lactation certifications (I'm a CLEC). Some are also massage therapists, and some are even Labor and Delivery Nurses too, Some are professional photographers!
We usually say that you should interview about 3 doulas and really go with your gut on who is going to make you and your support team feel the most comfortable.
Generally speaking, they all normally do at least one or two prenatal visits, attend the birth for it's entirety, and one postpartum visit.
What does a doula charge?
| - that's me and my daughters. My little one is holding a sign that says, "I'm improving birth because I had a doula." - that's the look on my face when I saw my doula at my wedding, for the first time since that birth. She's worth her weight in gold to me. I could never repay her for how much she has changed my life. I have my entire career to thank her inspiration for. I was more emotional seeing her than anyone else at my wedding. Seems crazy! But she was the most loving person and exactly what I needed. |
In this area there's a wonderful range of doulas and options. We have student doulas who might charge as little as $300 and even take payments. The more experienced, but still a little fresh doulas might charge more around $500-$600. More experienced, skilled, and proficient doulas charge more around $800-$1200. Some do packages where you can choose what kind of services they offer (for example, including photography or not) and that would create a range within their fees. Rarely, some insurance companies do cover birth doulas. You can use your HSA (health savings account) to pay for your doula if you have one. Although, I'm doing much less births than I used to, I will still interview with you, especially if you're my HypnoBirthing student! I charge $800. Otherwise, please allow me to help you find a doula who will fit your budget! I think EVERYONE deserves to have a doula!
So what happened when a doula, a midwife, and an OB walked into a bar?
They all talked about how amazing it is to witness the unpredictable, completely transformative, miracle of life. And they all had only one drink because who knows when the next 2am phone call would be.
If you read my last blog, now you understand what separates a midwife from an OB. But the conversation doesn't end there. You won't always get the exact same kind of care from midwife to midwife.
Not all midwives do hospital births, not all midwives do homebirths. Only CNMs (in California) can work in a hospital to deliver babies. Both can have a homebirth or birth center practice...
Here's why:
Certified Nurse Midwives become RNs before adding on about another couple years of education to earn their Midwife-status. Their education is usually within a typical college. As they become nurses first, they often hear about birth as described in the modern-medicine way. If they only ever work in a hospital, they might earn the slang natural-birthing community label "med-wife," if they practice no different than an OBGYN.
However, many CNMs maintain the midwife philosophy that birth is generally safe and natural left alone and respected physiologically. Sometimes, they become frustrated if they work in a hospital and find themselves creating their own homebirth practice or birth center. But, because of their RN background, they are generally more acceptable for insurance companies.
In the Temecula area, there is no known CNM who routinely attends homebirths. However, there are a few San Diego based CNMs who have been known to make exceptions now and then. Most Kaiser hospitals in southern CA use CNMs for the majority of their deliveries. CNMs can accept Tri Care Standard, this is why they are used at the military bases for most deliveries as well. There is a birth center in driving distance called Tree of Life and the CNMs there can take a variation of insurances including Tri Care, there is no co-pay for Tri Care standard moms. And they also have an agreement for hospital transfers with Encinitas where they can continue as the main care provider even after the transfer (as long as the birth is vaginal). CNMs are also used at the UCSD birth center in San Diego. This birth center is within a hospital, but the birth center is a separate floor and maintains a true birth center feel to it. The midwives there are incredibly impressive in the way that they maintain respectful, expectant management, evidence-based care. UCSD accepts many insurances including Medi-Cal. Not only does UCSD and the military hospitals all use CNMs, but they all also offer Nitrous Oxide as a pain-relief option.
However, many CNMs maintain the midwife philosophy that birth is generally safe and natural left alone and respected physiologically. Sometimes, they become frustrated if they work in a hospital and find themselves creating their own homebirth practice or birth center. But, because of their RN background, they are generally more acceptable for insurance companies.
In the Temecula area, there is no known CNM who routinely attends homebirths. However, there are a few San Diego based CNMs who have been known to make exceptions now and then. Most Kaiser hospitals in southern CA use CNMs for the majority of their deliveries. CNMs can accept Tri Care Standard, this is why they are used at the military bases for most deliveries as well. There is a birth center in driving distance called Tree of Life and the CNMs there can take a variation of insurances including Tri Care, there is no co-pay for Tri Care standard moms. And they also have an agreement for hospital transfers with Encinitas where they can continue as the main care provider even after the transfer (as long as the birth is vaginal). CNMs are also used at the UCSD birth center in San Diego. This birth center is within a hospital, but the birth center is a separate floor and maintains a true birth center feel to it. The midwives there are incredibly impressive in the way that they maintain respectful, expectant management, evidence-based care. UCSD accepts many insurances including Medi-Cal. Not only does UCSD and the military hospitals all use CNMs, but they all also offer Nitrous Oxide as a pain-relief option.
| *Water Birth Side note: Balboa Hospital, UCSD hospital, and Pomerado hospital all have tubs you are "allowed" to Labor in; however, they will tell you to get out at the time of birth. Their policies are birthing in the tub. Stand alone birth centers and homebirths are your only option if you want to actually birth in the water. |
A Certified Professional Midwife, or a Licensed Midwife are equally equipped for birth as much as a CNM. They are both trained, educated, and highly experienced medical professionals. From my perspective, they might even be MORE willing to resolve a challenge than rely on a quick-fix in the Operating Room. For example, they wouldn't so quickly look at a birth with a baby who's head was positioned difficultly for dissention and resolve to surgically remove the baby without trying to physically manipulate baby's position. In other words, home birth midwives in particular must be of the MOST skilled to handle challenges because they actually CANNOT rely on an OR at all. In the case of a true emergency, they will suggest a transfer to a hospital where an OBGYN will take over.
Some CPMs/LMs go to a school just for midwifery. The Nizhoni Institute of Midwifery is one of those schools and it's in San Diego. Others might do a different program but they all eventually take the NARM (national association of registered midwives) test which is regulated by the same medical board that regulates OBGYNs. LMs must also spend hundreds of hours working with an existing midwife as a predecessor. Sometimes they act in the role of the assistant as they learn. Sometimes the existing midwife works with another midwife as her assistant instead. From my experience in Southern California, most homebirth midwives work closely with other midwives and usually never attend a birth by themselves.
Although they are educated in Breech and Twin deliveries, they are legally restricted from delivering those babies. They also have legal restrictions in California to not provide care for a woman birthing earlier than 37 weeks or later than 42 weeks. Thankfully, they can still provide care for VBACs (vaginal births after cesarean). Hopefully there will be more freedoms for them as this political battle moves forward. On a better note, LMs now have the potential to accept Medi Cal! In this area, we have a wonderful midwife who accepts Medi Cal and her name is Cristi Lewis. She and another awesome midwife, Karen Pecora, are working on opening a birth center in Fallbrook called Acorn Midwifery. Keep in touch with Cristi (who also works as a Homeopath): http://highroadhomeopathy.com/About_Cristi_Lewis/index.html
There are different high risk variables that some midwives can still provide care for, there are some high risk variables that midwives would try and resolve naturally (for example, naturally lower blood pressure so a woman can get off medication), and there are other high risk complications that are best suited in the hands of an OBGYN in the hospital. Sometimes, parents chose to do co-care. This means they have both an OBGYN and a Homebirth Midwife. They know that the doctor is there if they need him/her but listen carefully to their midwives and do everything they can to not need them.
Some CPMs/LMs go to a school just for midwifery. The Nizhoni Institute of Midwifery is one of those schools and it's in San Diego. Others might do a different program but they all eventually take the NARM (national association of registered midwives) test which is regulated by the same medical board that regulates OBGYNs. LMs must also spend hundreds of hours working with an existing midwife as a predecessor. Sometimes they act in the role of the assistant as they learn. Sometimes the existing midwife works with another midwife as her assistant instead. From my experience in Southern California, most homebirth midwives work closely with other midwives and usually never attend a birth by themselves.
Although they are educated in Breech and Twin deliveries, they are legally restricted from delivering those babies. They also have legal restrictions in California to not provide care for a woman birthing earlier than 37 weeks or later than 42 weeks. Thankfully, they can still provide care for VBACs (vaginal births after cesarean). Hopefully there will be more freedoms for them as this political battle moves forward. On a better note, LMs now have the potential to accept Medi Cal! In this area, we have a wonderful midwife who accepts Medi Cal and her name is Cristi Lewis. She and another awesome midwife, Karen Pecora, are working on opening a birth center in Fallbrook called Acorn Midwifery. Keep in touch with Cristi (who also works as a Homeopath): http://highroadhomeopathy.com/About_Cristi_Lewis/index.html
There are different high risk variables that some midwives can still provide care for, there are some high risk variables that midwives would try and resolve naturally (for example, naturally lower blood pressure so a woman can get off medication), and there are other high risk complications that are best suited in the hands of an OBGYN in the hospital. Sometimes, parents chose to do co-care. This means they have both an OBGYN and a Homebirth Midwife. They know that the doctor is there if they need him/her but listen carefully to their midwives and do everything they can to not need them.
| What about the cost? One of the most daunting things about homebirth is the fact that most insurance companies do not realize how much money they could be saving if they covered more midwives! If you have a PPO, there's a chance you might only have a co-pay for your midwife. As mentioned earlier, medi-cal covers CPMs and Tri-Care standard covers CNMs. Sometimes you have to get a letter sent to your insurance company by a doctor or a midwife for them to approve you. Otherwise, it might be worth it to save up the $4000-$6000 needed to pay for your midwife. Remember, that covers ALL of your care! It's true, They don't get paid nearly enough. |
Often I'm asked what's the difference between a doula and a midwife. That question leads to an answer of much greater length then the one asking usually suspects. So, I decided to take a moment to describe all the information I'd like to share about all the different kinds of support person(s) and medical professionals you can have at your birth. I will address comparisons and contrasts throughout the next few blogs.
First, lets break down what the difference is between an OBGYN and a midwife. Yes, you will get a sense of my bias. I'm not going to sugar coat any of the facts. I'm not going to unsee what I have already seen.
First, lets break down what the difference is between an OBGYN and a midwife. Yes, you will get a sense of my bias. I'm not going to sugar coat any of the facts. I'm not going to unsee what I have already seen.
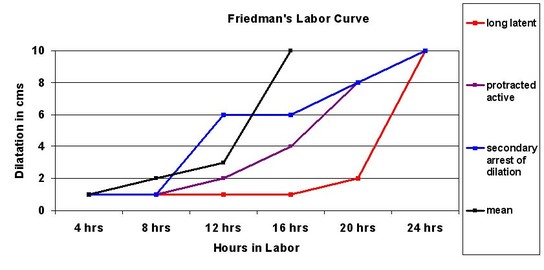 This unethical expectation put on women to progress in a certain amount of time, has ALREADY been debunked. Unfortunately, the culture build around it has grown over 50 years worth of improper care. It has become nearly impossibly to undo in the hospital setting.
This unethical expectation put on women to progress in a certain amount of time, has ALREADY been debunked. Unfortunately, the culture build around it has grown over 50 years worth of improper care. It has become nearly impossibly to undo in the hospital setting. Why do Doctors and Midwives practice so differently? Don't they both deliver babies? Is it really all just about money?
Let's take a deeper look...
| Both of these providers are qualified to provide prenatal care, antepartum (during labor) care, and postpartum care as well as the delivery of the baby. A midwife is qualified to handle any birth related occurrence apart from surgical birth. Only an OBGYN can perform cesareans. OBGYNs are trained to look for pathology. They look for what could go wrong and try to fix it before it could get "broken". Generally speaking, they are more comfortable with controlled management. They are not taught how emotional components affect labor. They have never been trained to provide care for natural births; rather, the interventions they can use to manage birth. Thanks to Dr. Freidman's Labor Curve (http://evidencebasedbirth.com/friedmans-curve-and-failure-to-progress-a-leading-cause-of-unplanned-c-sections/) of 1955, most OBGYNs still believe that there is a right way and a wrong way to progress in labor. Many of them have never seen a naturally occurring (spontaneous) labor that ended in a completely natural birth without intervention. In parts of the world where the cesarean rates are not outrageous midwives attend most of the births, and their cesarean rates are between 5% and 15%. Midwives look at birth as generally a naturally occurring experience that is works best unencumbered when women feel confident, safe, and comfortable. They're taught how to resolve any challenges without drugs; rather, natural methods. They never fix something that isn't broken. They are well educated on how the sympathetic nervous system offends the natural process and know how to calm a woman emotionally so her body can react physically better. They also know how to resolve emergencies with medical care and can use that only when truly necessary. Midwives are the leading providers for labor and delivery world wide. Midwives handle all healthy moms with healthy pregnancies in most of the world. Generally speaking, 95% of births are low risk. Where midwives are the ones treating the 95% of births, the outcomes are always better. Lower mortality for moms and babies, less cesareans, less interventions, less NICU stays. The United States has one of the highest mortality rates in all developed countries. Homebirth midwives only attend about 1% of the births in the U.S. Thankfully, we have organizations like Improving Birth (https://improvingbirth.org/) that are making strides at creating awareness for this problem. In the United States, Doctors have only been attending the majority of births for around about the last 85 years. When newspaper articles were printed with mass influence in the 1920s, families read that midwives were witches and hospitals were the safer and cleaner place to have babies. Because doctors were never trained on how to help women birth naturally, narcotics came about to knock women out. So, forceps were invented to deliver babies instrumentally since their mothers were out cold. This caused internal bleeding in baby's brains and it why we have the vitamin K shot today. (Vitamin k helps baby's blood clot so it can heal itself). Midwives (although there are different kinds) are trained to attend low risk births and handle them with expectant management. Again, that means that they don't fix what's not broken. And again, this kind of care applies to 95% of all births. Medically speaking, they do the same routine things during the birth like check the mother's vital signs, look for signs of infection, check the baby's heart rate, and vaginal exams. They take care of the mom. If the mom is tired, they show her how to get comfortable enough to sleep. If the mom is uncomfortable, they use techniques to physically comfort her and show her support persons how to also. If the baby is not properly positioned, they know how to get the baby into the right position. Many times this involves a lot of movement on the mother's part. Before they go to medical means, they try natural means to create a more safe and comfortable experience for the family. They know how to handle emergencies such as shoulder dystocia, resuscitation needed for baby or mom at birth, postpartum hemorrhaging. And they are capable of administering various drugs if needed. They can do IVs and they can repair a tear in the mother's perineum or elsewhere around the birth path. They cannot perform surgery. They bring oxygen and life-saving tools and medication with them if they're doing a home birth. However, rarely are those tools needed because the baby and mom are not experiencing any side affect of anesthetics or instrumental deliveries. |
1. Dr Stu - L.A. based doctor who does homebirths. This is your only (legal) option if you are having twins and want a home birth. He only accepts cash, no insurances. He is the only OB who does homebirths in a 60-mile radius.
2. Dr. Kenneth James - Laguna Hills
3. Dr. Cobb - Pomerado hospital in Poway (gets booked quickly! catch him early) This hospital has laboring tubs.
4. Dr. Capetanakis - Scripps Encinitas. Also known also for allowing skin to skin in the OR in the case of a necessary cesarean.
5. Dr. Vu - Sharp Grossmont (also privileges at Sharp Mary Birch). Best known for being highly skilled with Vaginal Breech deliveries.
6. If you are a Kaiser patient, you're best bet is to go to Zion in San Diego. That hospital compared to Palomar, Moreno Valley, and Riverside, has much more of a comfort with the natural birthing community. Usually the nurses are familiar with HypnoBirthing.
2. Dr. Kenneth James - Laguna Hills
3. Dr. Cobb - Pomerado hospital in Poway (gets booked quickly! catch him early) This hospital has laboring tubs.
4. Dr. Capetanakis - Scripps Encinitas. Also known also for allowing skin to skin in the OR in the case of a necessary cesarean.
5. Dr. Vu - Sharp Grossmont (also privileges at Sharp Mary Birch). Best known for being highly skilled with Vaginal Breech deliveries.
6. If you are a Kaiser patient, you're best bet is to go to Zion in San Diego. That hospital compared to Palomar, Moreno Valley, and Riverside, has much more of a comfort with the natural birthing community. Usually the nurses are familiar with HypnoBirthing.
Karen Brann
Birth Doula, Childbirth Educator, Lactation Educator/Counselor
Archives
July 2019
December 2017
November 2017
June 2017
January 2017
December 2016
September 2016
August 2016
July 2016
April 2016
March 2016
February 2016
January 2016
December 2015






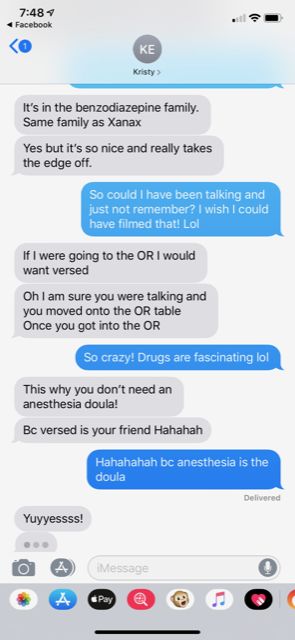











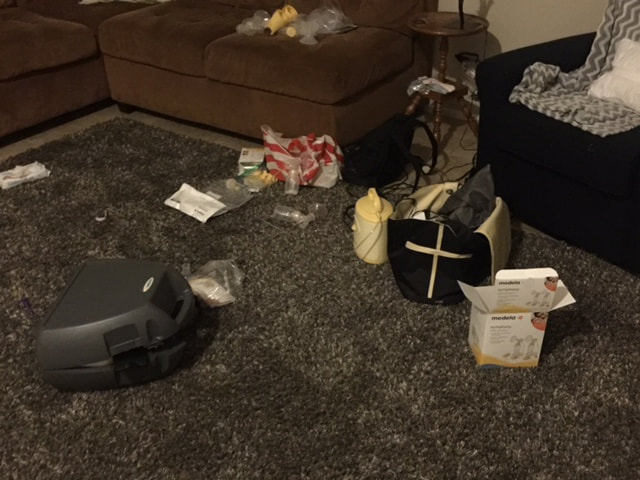







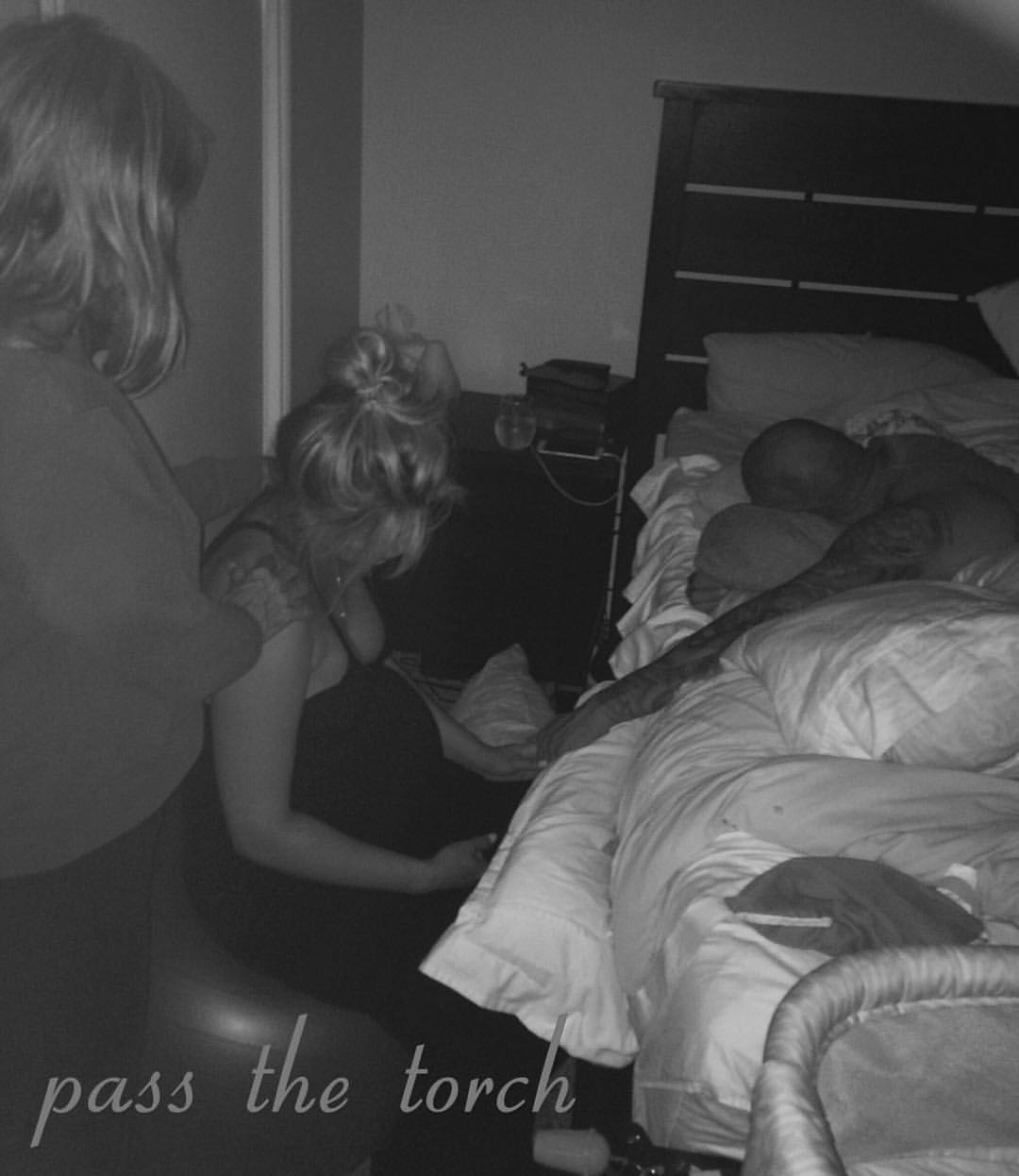



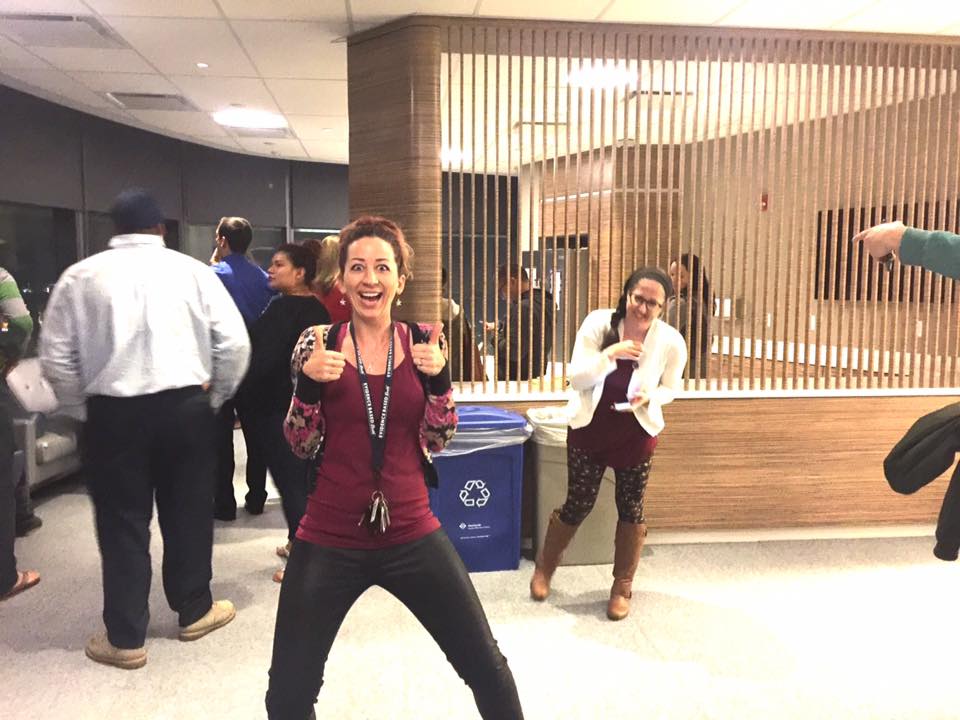
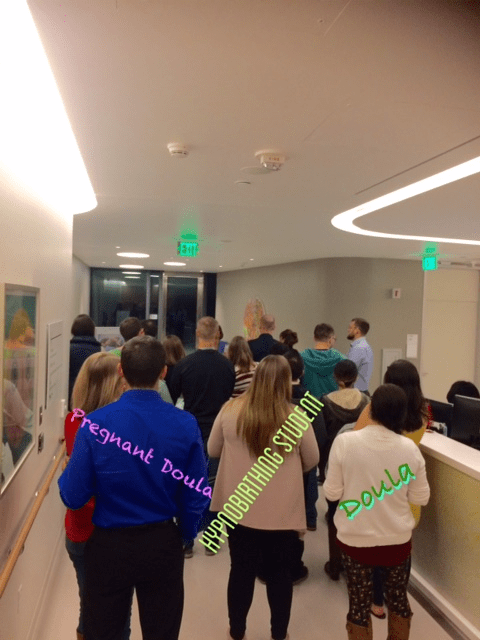
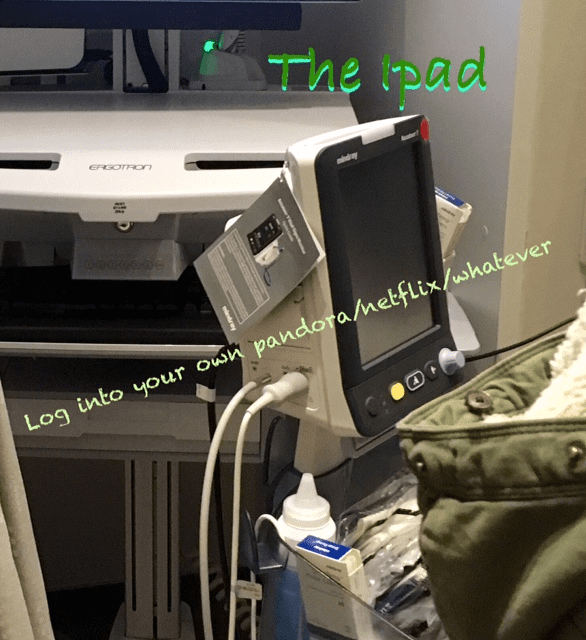
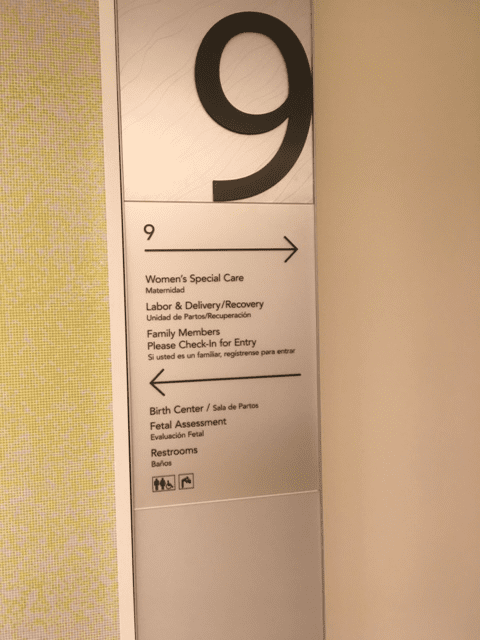


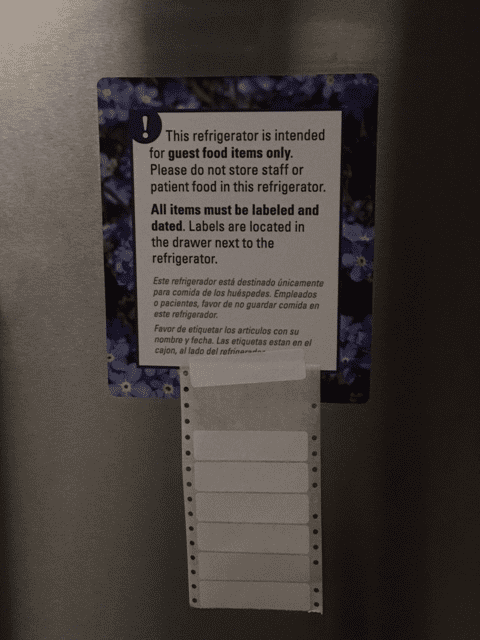







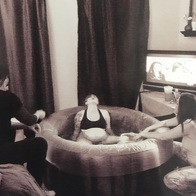






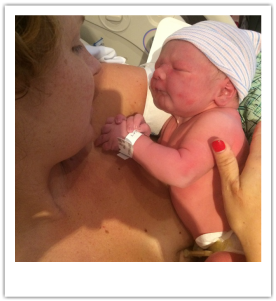
 RSS Feed
RSS Feed
